Good morning and greetings from
the Green Mountain State! 8/11/2022
With the 2022 Medicaid
Enterprise System Conference (MESC) just days away, Vermont is sending our
annual pre-conference communication. This allows us to maximize the
opportunities at MESC, to further build relationships, gain additional
information, and increase awareness about industry standards, best practices,
and lessons learned.
Vermont continues to follow guidance from our Federal
Partners and move forward with transforming our Medicaid Enterprise and serving
Vermonters in the most time efficient, secure and integrated
manner. Over the past year, we achieved two more Centers for
Medicare and Medicaid Services (CMS) Certifications, for Health Information
Exchange (HIE) and Electronic Visit Verification (EVV). This brings our
total to five with the other modules being: Pharmacy Benefit Management
(PBM) (Change Healthcare), Care Management module (Kepro (formerly eQHealth)),
and Provider Management Module (PMM) (Gainwell Technologies). Vermont is
leveraging the expertise of our Independent Verification and Validation
(IV&V) vendor (CSG Government Solutions) and our Procurement and Technical
Advisor (NTT Data) to validate our expectations and planning efforts and
continue our progress on our Medicaid Enterprise transformation.
Regarding Vermont’s
Enterprise:
- Medicaid Management Information
System (MMIS) Program:
- Note-1: Medicaid Data Lake and
Analytic Solution (MDLAS) procurement remains an active procurement and
we cannot discuss any aspect of that effort.
- Note-2: Vermont is interested
in scheduling MMIS Core Claims Processing Demonstrations and is expecting
MMIS vendors to speak to the following items. The state will
hold vendors to no more than an hour. Further details below
regarding what the State is looking to see and hear regarding your
MES/MMIS solution.
- Note-3: Clarity on Vermont’s
role as a public managed care entity.
- Vermont Medicaid does not contract
with traditional Managed Care Organizations (MCOs), nor does Vermont
operate in a purely Fee-for-Service model. Vermont has a publicly
operated non-risk Prepaid Inpatient Health Plan (PIHP) delivery model
through its 1115 demonstration waiver, whereby the state acts as a
public managed care entity. One component of the PIHP delivery
model is the ability to implement payment options available under a
managed care delivery structure. The Vermont Medicaid Next
Generation Accountable Care Organization (VMNG ACO) payment model is a
program for which a risk-bearing ACO receives a prospective payment and
assumes accountability for the costs and quality of care for
prospectively attributed Medicaid members. Therefore, Vermont
needs to report encounter data because payment is not contingent upon
fee-for-service billing.
- For more than a decade, Vermont has
engaged in ambitious Medicaid and multi-payer reform efforts, seeking to
develop advanced alternative payment models for Medicaid services that
provide incentives for care delivery reform and support value-based
care. In line with CMS’ State Medicaid Director’s Letter in 2020
that outlined a vision for value-based care opportunities in Medicaid,
Vermont has a robust portfolio of Medicaid payment reform initiatives.
Through the Health Care Payment Learning and Action Network, (HCP-LAN)
CMS has established a framework and targets for states to move from
traditional fee-for-service models to advanced alternative payment
models with quality components. Vermont Medicaid is leading the nation
with nearly 70% of Medicaid payments falling into an advanced
alternative payment model arrangement. As Vermont continues to
modernize the Enterprise, systems and technology that support these
policies and offer the flexibility to adapt, create, expand and evaluate
programs beyond traditional fee-for-service arrangements will be key
considerations.
- The Department of Vermont Health
Access (DVHA), on behalf of the Agency of Human Services (AHS),
administers the Medicaid Program. The graphic below depicts
the PIHP model and illustrates the role that DVHA plays for establishing
relationships across State Agencies/Departments and contractors to
deliver Medicaid services for Vermont’s members.

- Below are some additional examples
of what the state is looking to see and discuss.
- What
aspects of our Medicaid program business model cause issues for your
MES/MMIS?
- What
aspects of our Medicaid program business model would be supported by
your MES/MMIS?
- As you
discuss functionality, explain if the functionality is part of your
NASPO awarded offering (if applicable) or if this is new functionality
not included in their NASPO claims/financial module scope
- Is your
encounter engine able to stand-alone as a module and be integrated with
our vendors solutions?
- Ability to
receive encounter data (using the above example) from providers – both
Medicaid enrolled and not – and capture the key elements we need such
as:
- Member
- Service
information – amount, duration, number delivered
- Place of
service
- Dates of
service
- Social
Determinates of Health (SdoH) data if provided
- Ability
to capture a “Would Have Paid” amount reflecting what a service would
have otherwise cost for informational purposes and cost avoidance when
necessary.
- Sometimes
referred to as: Zero-paid claim, Encounter claim, or a Shadow
claim
- If using
claims to do this, then a way to allow these to travel down a different
path than a regular Medicaid claim with all of the checks, edits and
audits
- Ability
to easily distinguish Medicaid / non-Medicaid in terms of services
delivered in a program with mixed attribution – easily reported
separately and together
- Benefit
package flexibility
- Ability
to create programs with services via a configurable mechanism
- Who
(State, vendor) typically does this work and what role (BA, Tech,
etc.)?
- Ability
to include / exclude benefits, services from the Medicaid Total Cost of
Care
- Ability
to adjust attribution of members to programs
- Easier
linking of members and providers to these different benefit packages
and programs
- Easy way
to change rates in the system for services with one-to-many
relationships with different programs
- Ability
to adjudicate claims funded by multiple federal and state funding
sources per hierarchy established by federal and state payor of last
resort regulation
- Updated
Financial module that allows for easier tracking of value-based
purchasing arrangements with providers
- Bundles
- PMPMs
- Case
rates, including tiers
- Special
program payments
- Review
of Reimbursement Methodology – how flexible is your solution with
regard to the procedures and adding codes to pay for new services such
as housing or fuel
- Additional
solution flexibility to address COVID-19 waiver, 1115 Waiver, and the
upcoming unwinding activities related to members and providers
- Integrated Eligibility and Enrollment
(IE&E) Program:
- Vermont has a number of IE&E
efforts that will result in procurement opportunities. The next
effort will be a Request for Proposals (RFP) for addressing noticing
needs for the Agency of Human Services (AHS)
- Health Information Exchange (HIE)
Program:
- Has started various initiatives
related to establishing Data Governance for AHS
- Key stakeholders have met to discuss
our modernization efforts and the future role HIE plays to address SdoH
We look forward to engaging
attendees and discussing your creative visions and new ideas as we continue the
build out of our Medicaid Enterprise. We are looking for experienced and
proven partners that are innovators and visionaries. We want to hear
where you recently have been implementing solutions and we are interested in
learning more about sharing and integrating technologies/capabilities across
our programs. We want to know the good and the challenging aspects you’ve
encountered. As identified in CMS’ Seven Standards and Conditions, we
desire solutions, services and components that are flexible, scalable and can
be leveraged/shared across boundaries.
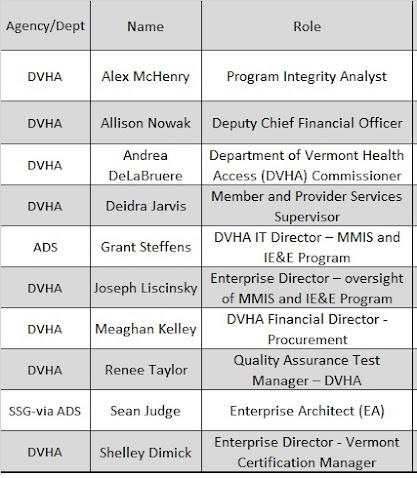
Vermont staff attending MESC
include the following: