The Department of Vermont Health Access is excited to announce that a contract was executed with Berry, Dunn, McNeil & Parker, LLC to provide Medicaid Enterprise consulting and procurement assistance. The State of Vermont will leverage BerryDunn's) experience and expertise, and their Transform Health and Human Services (tHHS) product to support Enterprise Modernization efforts across the Medicaid Management Information System (MMIS), Integrated Eligibility & Enrollment (IE&E), and Health Information Technology/Exchange (HIT/HIE) Programs.
State of Vermont - AHS/DVHA Communication
Welcome to the State of Vermont Agency of Human Services (AHS) and Department of Vermont Health Access (DVHA) communication blog. The State utilizes this site to share a clear and consistent message regarding AHS and DVHA major initiatives to any and all interested parties. This blog is updated on a periodic basis and you can follow it here directly or be alerted to it by receiving our twitter messages (@DVHAVermont). Thank you for your interest.
Monday, January 20, 2025
DVHA announces Medicaid Enterprise consulting and procurement assistance contract
Friday, October 13, 2023
Vermont - IE&E Modernization Update
|
Thursday, September 28, 2023
Vermont posts two RFP - Analytics Data Warehouse (ADW) and Security as a Service (SECaaS)
Monday, August 14, 2023
Vermont's 2023 - Pre-MESC Update
We’re only
days away from the 2023 Medicaid Enterprise System Conference (MESC) and we
know you’ve been anxiously awaiting Vermont’s annual pre-conference communication. This allows us to maximize the opportunities
at MESC, to further build relationships, gain additional information, and
increase awareness about industry standards, best practices, and lessons
learned.
Vermont
continues to move forward with transforming its Medicaid Enterprise and serving
Vermonters in the most time efficient, secure and integrated manner. Vermont has five Centers for Medicare and
Medicaid Services (CMS) Certified modules:
Health Information Exchange (HIE) (Vermont Information Technology
Leaders (VITL)), Electronic Visit Verification (EVV) (Gainwell & Sandata), Pharmacy
Benefit Management (PBM), (Change Healthcare), Care Management module (Acentra
Health (formerly Kepro (formerly eQHealth))), and Provider Management Module
(PMM) (Gainwell Technologies). Vermont
is leveraging the expertise of our Independent Verification and Validation
(IV&V) vendor (CSG Government Solutions) as we continue our Medicaid
Enterprise transformation.
Regarding Vermont’s Enterprise:
v Medicaid Management Information System (MMIS) Program:
o
Note-1: Medicaid Data Lake and Analytic Solution
(MDLAS) procurement was awarded to Deloitte and executed in July 2023.
o
Note-2: Vermont will be releasing a Request for
Proposals (RFP) for an Analytics Data Warehouse (ADW) to be implemented and will
integrate with our MDLAS. Be advised the
ADW will be maintained by Vermont’s HIE.
o
Note-3: Vermont Medicaid is not a traditional Managed
Care Organization (MCO), a traditional Accountable Care Organization (ACO), nor
all Fee-for-Service. Vermont runs a
publicly operated PIHP (Prepaid Inpatient Health Plan) delivery model
through its 1115 demonstration waiver.
One component of the PIHP delivery model is the ability to implement payment
options available under a managed care delivery structure. The Vermont
Medicaid Next Generation ACO (VMNG ACO) payment model is a program for which a
risk-bearing Accountable Care Organization (ACO) receives a prospective payment
and assumes accountability for the costs and quality of care for prospectively
attributed Medicaid members. Therefore, Vermont must report encounter
data for both traditional medical and Home and Community Based (HCBS) or Long-Term
Services and Supports (LTSS) programs because encounter data doesn't fall into
traditional reporting protocols.
v
Vermont is interested in scheduling MMIS Core Solution Demonstrations.
Context and expectations for those demonstrations follow below.
o
Vermont’s MMIS Core
Claims reprocurement approach:
§ MMIS Procurement Assistance RFP: Vermont will release
an RFP for services to work with VT MMIS staff to deliver a cost-benefit
analysis, roadmap, and an MMIS Claims and Fiscal Agent (FA) Services (MMIS
& FA) RFP. MMIS Procurement Assistance
RFP to be released this calendar year.
§ MMIS & FA RFP: The timing of
this re-procurement is TBD. This MMIS & FA RFP will leverage NASPO with added details to address Vermont-specific needs. It's
these specific needs (some identified further below) that we are interested
in hearing at MESC about how vendor solutions can support them.
o
Vermont wants to hear
from MMIS solution vendors and see just how configurable your MMIS solution is
for implementing Vermont-specific needs. We realize an hour can limit what can
be covered but at a minimum SoV would set up time for vendors to cover the
following:
§ Your current “go-to-market” solution:
· What's it called and when was it CMS Certified?
· Where are you actively implementing this solution right
now?
· What is your average implementation time?
§ Show how configurable the system is for implementing any
changes associated with Encounter claims for ACO or HCBS/LTSS programming (aka
$0 paid claims)
§ Using the example above, show the system’s ability to
receive encounter data from Medicaid enrolled and non-Medicaid enrolled providers
focusing on how the system captures and displays key elements such as:
§
Member
§
Service information – amount, duration, number
delivered
§
Place of service
§
Dates of service
§
Social Determinants of Health (SDoH) data if provided.
§
Ability to use ‘shadow’ nature of the service –
delivered but paid $0 because the provider is being paid differently (e.g., a
bundled payment or a PMPM) but to capture a Would Have Paid amount,
based on codes, so that we can track what the service would have otherwise
cost, and do cost avoidance if necessary.
§
If using claims to do this, then a way to allow
these to travel down a different path than a regular Medicaid claim with all of
the checks, edits and audits.
§
Ability to easily distinguish Medicaid /
non-Medicaid in terms of services delivered in a program with mixed attribution
– easily reported separately and together.
o
Benefit package flexibility
§
Ability to create programs with services via a
configurable mechanism.
§
Ability to include / exclude benefits, services
from the Medicaid Total Cost of Care
§
Ability to adjust attribution of members to programs.
§
Easier linking of members and providers to these
different benefit packages and programs
§
Easy way to change rates for services with
one-to-many relationships with different programs.
o
Financial module allowing for easier tracking of
value-based purchasing arrangements with providers.
§
Bundles
§
PMPMs
§
Case rates, including tiers.
§
Special program payments
§
Review of Reimbursement Methodology – how
flexible is your solution with regard to the procedures and adding codes to pay
for new services such as housing.
o
Additional
solution flexibility to address COVID-19 waiver, 1115 Waiver, and the upcoming
unwind activities related to members and providers.
o
Ability to integrate with
provider information, including demographics and patient population.
The following are additional
details of other Vermont related efforts:
v Integrated Eligibility and Enrollment (IE&E) Program:
o
Vermont has engaged in multiple Requests for Information (RFI) to increase
the collaboration and exchange of information with the vendor community.
- Vermont’s IE&E Program Team is pursuing a
“Prime” vendor to implement a "customer-focused" core system
that includes a Customer Portal, Case Management, and Business Rules
Engine while taking advantage – where possible – of existing technologies
to meet our end-to-end customer experience needs. This effort is called
the Vermont Integrated Eligibility System (VT-IES).
- The VT-IES (pronounced VEE-Ties) Project
will optimize eligibility, enrollment, and benefits management
functionality to allow Vermonters to apply for, receive, and manage
health coverage and economic assistance benefits through a user-centric
access point that is personalized, welcoming & comprehensive.
o
VT-IES is an integral
component of Vermont’s IE&E System Modernization efforts and will work
alongside the IE&E Noticing Project to simplify the process of
applying for and managing healthcare and financial benefits for Vermonters.
o
The VT-IES Project is in
the final stage of RFP development and is supported by NTT DATA. The RFP is
slated for release during 4th calendar quarter of 2023.
o
For additional information
on VT-IES, please visit Integrated Eligibility and
Enrollment (IE&E) System | Agency of Human Services (vermont.gov)
v Health Information Exchange (HIE) Program:
o
Has started various
initiatives related to establishing Data Governance for AHS
o
Key stakeholders
have met to discuss our modernization efforts and the future role HIE plays to
address Social Determinants of Health (SDoH)
v
Systems
Testing workgroup – as you may recall
from last year, Vermont, with the support of NESCSO, has established this
workgroup to discuss and review best practices for User Acceptance Testing,
Section 508 Compliance, Testing Maturity, Testing Automation, and more. The next System Testing workgroup meeting
will be held September 21, 2023. If you are interested in joining, please sign
up here. (State and State
partners only, please). This workgroup
has been working with TransformHHS (tHHS) on their workgroup page and State
Health Dashboard (SHD). If you have any
questions, please contact Vermont’s Quality Testing Director, Renee Taylor, at renee.taylor@vermont.gov.
v
Certification
workgroup – as you may recall from last
year, Vermont, with the support of CMS, Shelley Dimick, Vermont’s Certification
Director, has established a national Certification workgroup to support State
Medicaid Agencies collaboration. This workgroup shares best practices,
lessons learned, and provides clarity related to CMS Certification policies and
workflows. Tuesday (8/22) morning, Shelley will be having an in-person S-TAG
Certification meeting over breakfast at 8:30. If you are interested in
joining this workgroup of if you have any questions, please contact Shelley at Shelley.Dimick@vermont.gov.
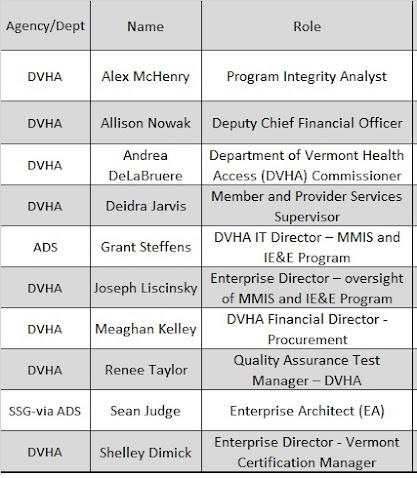
Vermont staff attending MESC include the following:
We look forward to our interaction during MESC - safe travels and see you in Denver!
Saturday, October 29, 2022
State of Vermont Announces Release of Independent Verification and Validation (IV&V) Request for Proposals (RFP)
Good morning everyone and greetings from the great Green Mountain State!
The State of Vermont, Agency of Human Services (AHS), Department of Vermont
Health Access (DVHA) is excited to announce the posting of an Independent
Verification and Validation (IV&V) Request for Proposals (RFP).
We are seeking to establish a contract with a vendor to provide IV&V
services associated with the modernization of the State’s Medicaid Enterprise
System (MES).
The RFP can be accessed at the following link: http://www.vermontbusinessregistry.com/BidPreview.aspx?BidID=57122
NOTE: when accessing this web-page there are two links on this web-posting:
- 1State of Vermont IVV-QA
RFP 03410-200-23.docx: will open the
RFP doc itself
- 'Independent
Verification and Validation RFP 03410-200-23 Bi: this is the
bid response template and be advised we are currently having an issue with
the link.
As a reminder, tell your family and friends of our blog (http://vermont-ahs-dvha.blogspot.com/)and
twitter (@DVHAVermont) account
to stay informed of what’s happening with our modernization efforts.
Have a great day and weekend.
Thursday, August 11, 2022
Vermont MMIS Update prior to MES Conference
Good morning and greetings from
the Green Mountain State! 8/11/2022
Regarding Vermont’s Enterprise:
- Medicaid Management Information
System (MMIS) Program:
- Note-1: Medicaid Data Lake and
Analytic Solution (MDLAS) procurement remains an active procurement and
we cannot discuss any aspect of that effort.
- Note-2: Vermont is interested
in scheduling MMIS Core Claims Processing Demonstrations and is expecting
MMIS vendors to speak to the following items. The state will
hold vendors to no more than an hour. Further details below
regarding what the State is looking to see and hear regarding your
MES/MMIS solution.
- Note-3: Clarity on Vermont’s
role as a public managed care entity.
- Vermont Medicaid does not contract
with traditional Managed Care Organizations (MCOs), nor does Vermont
operate in a purely Fee-for-Service model. Vermont has a publicly
operated non-risk Prepaid Inpatient Health Plan (PIHP) delivery model
through its 1115 demonstration waiver, whereby the state acts as a
public managed care entity. One component of the PIHP delivery
model is the ability to implement payment options available under a
managed care delivery structure. The Vermont Medicaid Next
Generation Accountable Care Organization (VMNG ACO) payment model is a
program for which a risk-bearing ACO receives a prospective payment and
assumes accountability for the costs and quality of care for
prospectively attributed Medicaid members. Therefore, Vermont
needs to report encounter data because payment is not contingent upon
fee-for-service billing.
- For more than a decade, Vermont has
engaged in ambitious Medicaid and multi-payer reform efforts, seeking to
develop advanced alternative payment models for Medicaid services that
provide incentives for care delivery reform and support value-based
care. In line with CMS’ State Medicaid Director’s Letter in 2020
that outlined a vision for value-based care opportunities in Medicaid,
Vermont has a robust portfolio of Medicaid payment reform initiatives.
Through the Health Care Payment Learning and Action Network, (HCP-LAN)
CMS has established a framework and targets for states to move from
traditional fee-for-service models to advanced alternative payment
models with quality components. Vermont Medicaid is leading the nation
with nearly 70% of Medicaid payments falling into an advanced
alternative payment model arrangement. As Vermont continues to
modernize the Enterprise, systems and technology that support these
policies and offer the flexibility to adapt, create, expand and evaluate
programs beyond traditional fee-for-service arrangements will be key
considerations.
- The Department of Vermont Health
Access (DVHA), on behalf of the Agency of Human Services (AHS),
administers the Medicaid Program. The graphic below depicts
the PIHP model and illustrates the role that DVHA plays for establishing
relationships across State Agencies/Departments and contractors to
deliver Medicaid services for Vermont’s members.
- Below are some additional examples
of what the state is looking to see and discuss.
- What
aspects of our Medicaid program business model cause issues for your
MES/MMIS?
- What
aspects of our Medicaid program business model would be supported by
your MES/MMIS?
- As you
discuss functionality, explain if the functionality is part of your
NASPO awarded offering (if applicable) or if this is new functionality
not included in their NASPO claims/financial module scope
- Is your
encounter engine able to stand-alone as a module and be integrated with
our vendors solutions?
- Ability to
receive encounter data (using the above example) from providers – both
Medicaid enrolled and not – and capture the key elements we need such
as:
- Member
- Service
information – amount, duration, number delivered
- Place of
service
- Dates of
service
- Social
Determinates of Health (SdoH) data if provided
- Ability
to capture a “Would Have Paid” amount reflecting what a service would
have otherwise cost for informational purposes and cost avoidance when
necessary.
- Sometimes
referred to as: Zero-paid claim, Encounter claim, or a Shadow
claim
- If using
claims to do this, then a way to allow these to travel down a different
path than a regular Medicaid claim with all of the checks, edits and
audits
- Ability
to easily distinguish Medicaid / non-Medicaid in terms of services
delivered in a program with mixed attribution – easily reported
separately and together
- Benefit
package flexibility
- Ability
to create programs with services via a configurable mechanism
- Who
(State, vendor) typically does this work and what role (BA, Tech,
etc.)?
- Ability
to include / exclude benefits, services from the Medicaid Total Cost of
Care
- Ability
to adjust attribution of members to programs
- Easier
linking of members and providers to these different benefit packages
and programs
- Easy way
to change rates in the system for services with one-to-many
relationships with different programs
- Ability
to adjudicate claims funded by multiple federal and state funding
sources per hierarchy established by federal and state payor of last
resort regulation
- Updated
Financial module that allows for easier tracking of value-based
purchasing arrangements with providers
- Bundles
- PMPMs
- Case
rates, including tiers
- Special
program payments
- Review
of Reimbursement Methodology – how flexible is your solution with
regard to the procedures and adding codes to pay for new services such
as housing or fuel
- Additional
solution flexibility to address COVID-19 waiver, 1115 Waiver, and the
upcoming unwinding activities related to members and providers
- Integrated Eligibility and Enrollment
(IE&E) Program:
- Vermont has a number of IE&E
efforts that will result in procurement opportunities. The next
effort will be a Request for Proposals (RFP) for addressing noticing
needs for the Agency of Human Services (AHS)
- Health Information Exchange (HIE)
Program:
- Has started various initiatives
related to establishing Data Governance for AHS
- Key stakeholders have met to discuss
our modernization efforts and the future role HIE plays to address SdoH
We look forward to engaging
attendees and discussing your creative visions and new ideas as we continue the
build out of our Medicaid Enterprise. We are looking for experienced and
proven partners that are innovators and visionaries. We want to hear
where you recently have been implementing solutions and we are interested in
learning more about sharing and integrating technologies/capabilities across
our programs. We want to know the good and the challenging aspects you’ve
encountered. As identified in CMS’ Seven Standards and Conditions, we
desire solutions, services and components that are flexible, scalable and can
be leveraged/shared across boundaries.
Vermont staff attending MESC
include the following:
Wednesday, January 26, 2022
Vermont announces posting of Medicaid Data Lake and Analytic Solutions (MDLAS) Request for Proposal (RFP)
Good afternoon everyone and greetings
from the great Green Mountain State.
Vermont’s Agency of Digital Services (ADS), the Agency of Human Services (AHS),
and the Department of Vermont Health Access (DVHA) are excited to announce the
posting of a Request for Proposal (RFP) to contract for Vermont’s Medicaid Data
Lake and Analytic Solutions (MDLAS).
This is part of the State’s larger effort for our Medicaid Data
Warehouse and Analytic Solution (MDWAS).
This RFP is located at: Department
of Buildings & General Services (state.vt.us).
Have a great day. Stay warm!
Thanks